Researchers at the University of Colorado Boulder have discovered a brain signature that identifies fibromyalgia (FM) patients with 93 percent accuracy. The discovery opens possibilities for improved fibromyalgia diagnosis and treatments in the future.
The report, “Towards a neurophysiological signature for fibromyalgia,” was published in the journal Pain.
Fibromyalgia (FM) is a condition characterized by widespread musculoskeletal pain accompanied by fatigue, sleep, memory, and mood issues. Patients with FM show enhanced reaction to painful and non-painful sensations that are accompanied by altered neural responses.
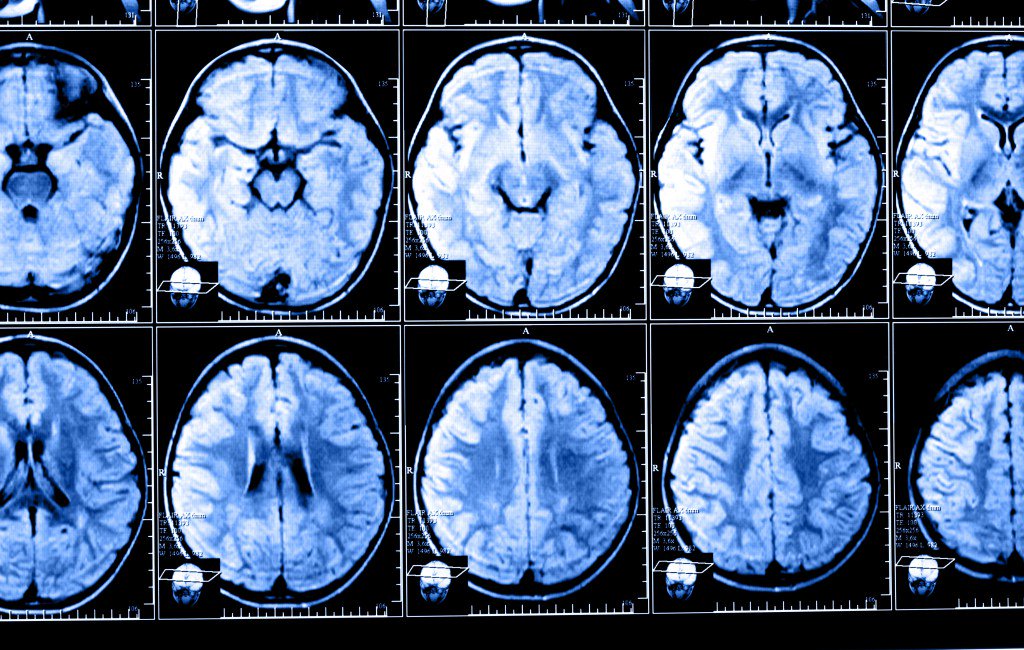
Using functional magnetic resonance imaging (fMRI), the researchers performed brain scans on 37 FM patients and 35 healthy controls. All subjects were exposed to painful pressure and non-painful visual, auditory, and tactile cues during the scans.
Computerized machine-learning techniques allowed the researchers to identify a brain-based FM signature. Specifically, when exposed to the same painful stimuli as people in the healthy control group, FM patients showed greater neurologic pain signature responses. The method relies on a computer algorithm developed by CU Bolder researchers to recognize a complex pattern of neuronal activation in the brains of subjects exposed to pain.
Researchers found that FM patients had increased responses in three sub-markers, which correlated with hypersensitivity to pain characterized by the condition. When researchers combined the neural signature methods, they were able to classify FM patients from controls with 92 percent sensitivity and 94 percent specificity.
“The novelty of this study is that it provides potential neuroimaging-based tools that can be used with new patients to inform about the degree of certain neural pathology underlying their pain symptoms,” Marina López-Solà, a post-doctoral researcher in the university’s Cognitive and Affective Control Laboratory and the lead author of the study, said in a news release.
The tools also provided an initial characterization of individual FM patients based on pathophysiological, symptom-related brain features. Results can help physicians place patients more accurately into subtypes and provide individualized treatments.
“Though many pain specialists have established clinical procedures for diagnosing fibromyalgia, the clinical label does not explain what is happening neurologically and it does not reflect the full individuality of patients’ suffering,” Tor Wager, director of the laboratory said. “The potential for brain measures like the ones we developed here is that they can tell us something about the particular brain abnormalities that drive an individual’s suffering. That can help us both recognize fibromyalgia for what it is – a disorder of the central nervous system – and treat it more effectively.”










